Rethinking Low Back Pain: A Lesson from Tendinopathy
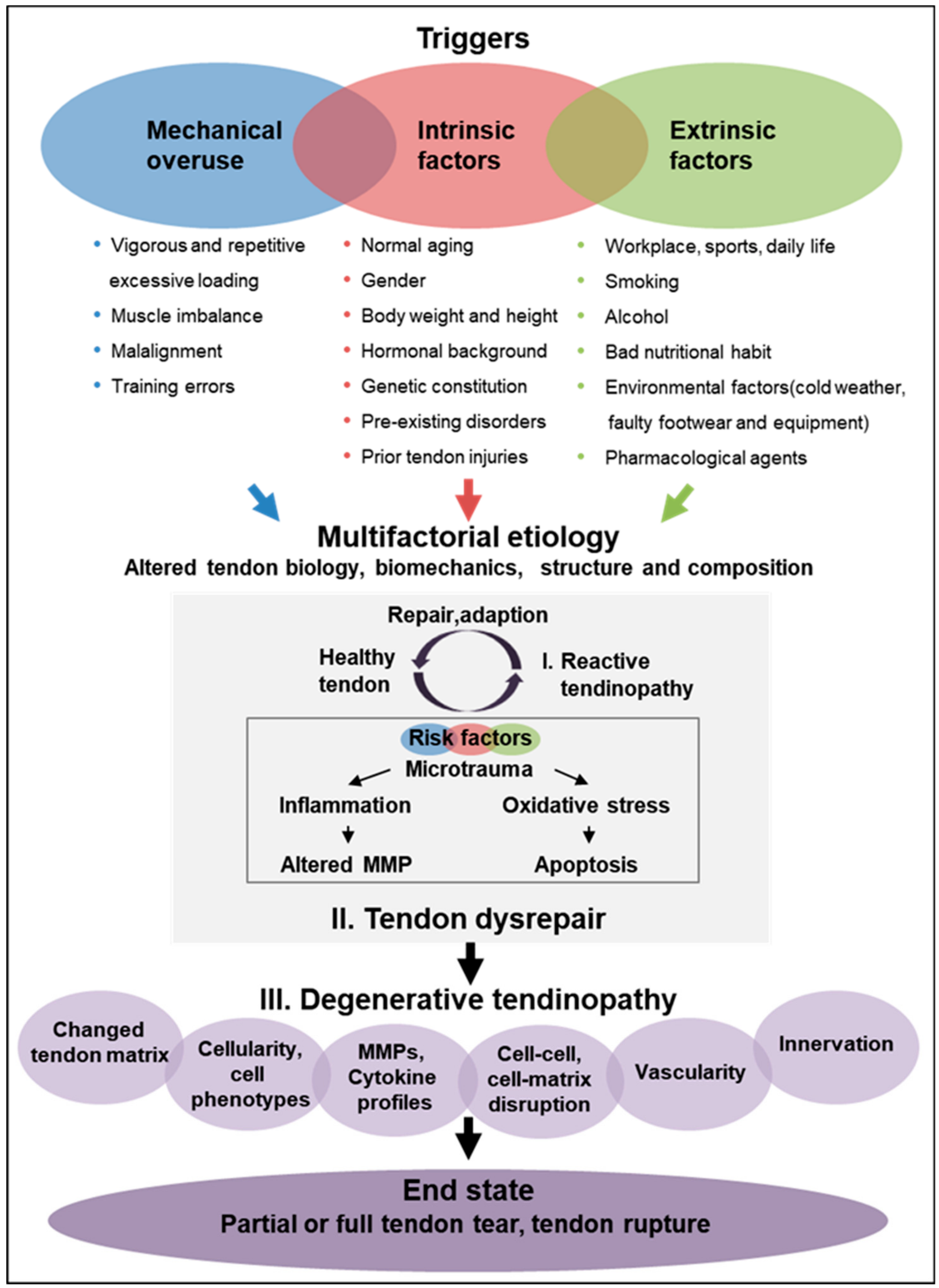
The conventional approach to treating low back pain with a "fix it" mentality may not always be adequate, especially for chronic conditions like low back pain. To truly address the intricacies of musculoskeletal disorders, a shift towards long-term management strategies is necessary. One valuable lesson we can learn is from the progressive model used in tendinopathy rehabilitation. Tendinopathy, a frustrating condition affecting tendons, was once treated with rest and anti-inflammatory medications, assuming inflammation was the core issue. However, this approach often led to recurrent symptoms upon resuming activity. By understanding that tendinopathy is primarily a degenerative condition involving structural and compositional changes in the tendon, clinicians were able to make a breakthrough in managing this condition. Similarly, we can better treat chronic low back pain by adopting a broader perspective and focusing on long-term management strategies.
Rehabilitation, whether it be for tendon issues or low back pain, requires a multi factored approach. In most cases there is not one specific cause, meaning we can create marginal gains by improving several different factors, which will add up to larger improvements.
The shift in understanding is crucial and has far-reaching implications in healthcare. By recognizing that many conditions, including tendinopathy and low back pain, are complex and multifactorial, healthcare professionals can develop more effective rehabilitation plans that focus on addressing the underlying causes of the issue rather than just treating the symptoms. This approach not only leads to better long-term outcomes but also helps to avoid the frustration and expense of repeated interventions that fail to solve the underlying problem. So, it's time to shift our mindset from "fix it" to "understand it and work with it."
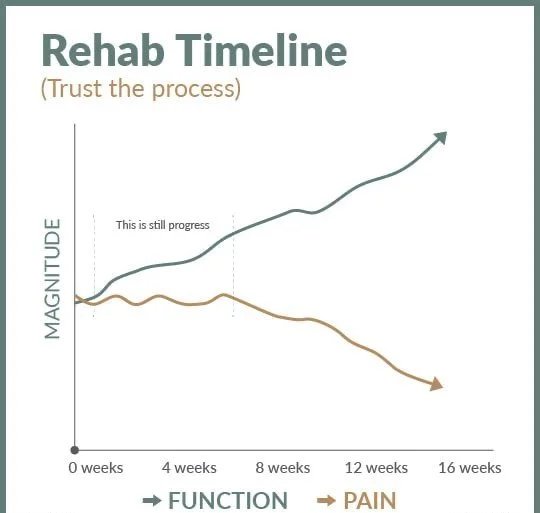
Pain is not the most reliable outcome measure. We must focus on improving function. With improved function over time will lead to improved pain tolerance. Trust the Process.
Healthcare providers, as the key facilitators of this shift, play a crucial role in educating patients about the benefits of long-term management strategies. By emphasizing the importance of gradually increasing load and activity, tailored exercises, and lifestyle changes, healthcare professionals can empower patients to take an active role in their recovery and prevent the recurrence of symptoms. This approach promotes physical healing and fosters resilience and adaptability in patients, thereby improving overall wellness and quality of life.
The shift from a "fix it" to a "manage it" approach in treating low back pain is a much-needed paradigm shift in the healthcare system. By adopting a long-term management approach similar to that used in tendinopathy, patients are better equipped to handle fluctuations in their symptoms and less likely to undergo unnecessary and invasive treatments that may have limited long-term effectiveness. This emphasis on long-term benefits can instill a sense of hope and optimism in the audience, knowing that there are effective strategies for managing their condition in the long run. This can help patients feel more positive and hopeful about their recovery journey.
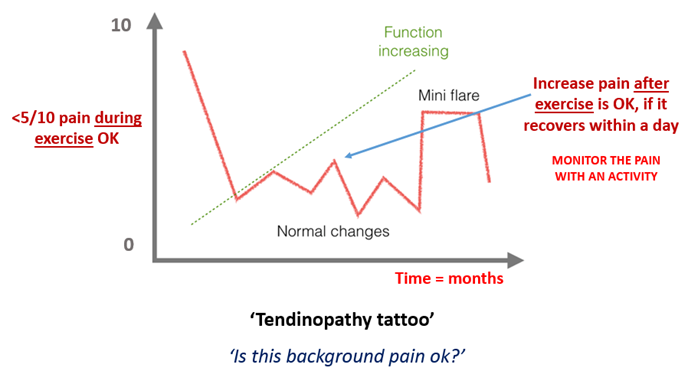
Pain and flares are normal during the rehabilitation process, we are more concerned that the overall slope of recovery remains positive.
This change in philosophy aligns more closely with the biological realities of chronic musculoskeletal conditions. It promotes a healthier, more sustainable relationship between patients and their bodies, encouraging them to be proactive and resilient instead of reactive and frustrated. The future of effective treatment for low back pain lies in a holistic, long-term management approach inspired by advances in tendinopathy rehabilitation.
Encouraging patient participation in their own care is a crucial aspect of managing low back pain through the lens of tendinopathy rehabilitation. This approach improves the effectiveness of clinical interventions. It profoundly impacts the patient's long-term health outcomes and relationship with chronic pain. By empowering patients to take an active role in their treatment, we can increase the impact of our efforts to manage low back pain and pave the way for better health outcomes. This sense of empowerment can make patients feel more in control of their condition and more proactive in their recovery journey.
Excessive load leads to further degeneration, we have to find the appropriate loads to stimulate the positive adaptive process.
Empowering Self-Management
Active patient participation begins with education. Patients who understand the nature of their condition and the principles behind their treatment options are more likely to engage actively in their management plan. For low back pain, this means explaining the non-linear nature of pain, the importance of physical activity for recovery, and how lifestyle factors influence symptoms. This educational component is akin to what is seen in tendinopathy rehabilitation, where patients learn about the biological processes of tendon adaptation and how exercise facilitates this change. This emphasis on understanding can make the audience feel more informed and knowledgeable about their condition and its management, fostering a sense of empowerment and confidence.
Structured Exercise Programs
Just as in tendinopathy, where specific loading programs are designed to gradually strengthen the affected tendon, patients with low back pain benefit from structured exercise programs tailored to their particular needs. These are not generic back exercises but are personalized based on a thorough clinical assessment, patient history, and individual capabilities. The focus on controlled, progressive loading helps to build resilience in the spinal structures, similar to how tendons adapt and strengthen.
The bridge between the current capacity and required capacity required patience, to gradually improve load tolerance.
Integration of Behavioral Strategies
Chronic low back pain is often intertwined with psychological factors such as anxiety, depression, and fear of movement (kinesiophobia). Integrating cognitive-behavioral strategies into the treatment plan addresses these aspects, encouraging a healthier mental approach to dealing with pain. Techniques might include pain coping skills training, mindfulness-based stress reduction, and cognitive-behavioral therapy, all aimed at modifying the patient's emotional and behavioral responses to pain.
Regular Monitoring and Adaptation
Active participation also means regularly monitoring one's progress and adapting the management plan as needed. This dynamic process, which involves both the clinician and the patient, is a cornerstone of effective management. For example, as a patient's strength and mobility improve, exercises can be progressively advanced to continue to challenge the body appropriately. Conversely, setbacks are managed by adjusting activity levels and integrating other therapeutic modalities. This ongoing adjustment aligns the treatment with the patient's current status, encouraging continual engagement and motivation.
The “Goldilocks Principle” applies to load management… not too much and not too little.
Long-Term Lifestyle Changes
Finally, active participation extends beyond the clinic. Patients are encouraged to integrate what they have learned into daily life. This could mean ergonomic adjustments at work, regular stretching routines at home, or lifestyle changes such as weight management and quitting smoking. Such changes are crucial for managing symptoms, improving overall health, and preventing future pain episodes.
“Recovery is about Landmarks not Timelines”
By fostering active participation in their care, patients with low back pain can achieve better outcomes, much like those managing tendinopathy. This approach helps patients move from feeling passive and dependent on medical interventions to being empowered and self-reliant. It promotes a deep, personal engagement with health that is both transformative and sustainable, setting a new standard in managing chronic conditions. The ultimate goal is to shift the paradigm from episodic care to continuous self-improvement, creating a culture of health that lasts a lifetime.